Treatment of glomus tumors with cyberknife.
INTRODUCTION
Glomus tumors, also known as paragangliomas, are benign, slowgrowing tumors, originating from neuroectodermal tissues. They are highly vascular lesions and arise from the capillary and precapillary blood vessels, located along the tympanic branch of glossopharyngeal nerve (Jacobson’s nerve). It occur predominantly in women, and are typically diagnosed between the fifth and sixth decade of life. Clinical aspects present as pulsatile tinnitus followed by conductive hearing loss, otalgia, and aural fullness.
METHERIALS AND METHODS
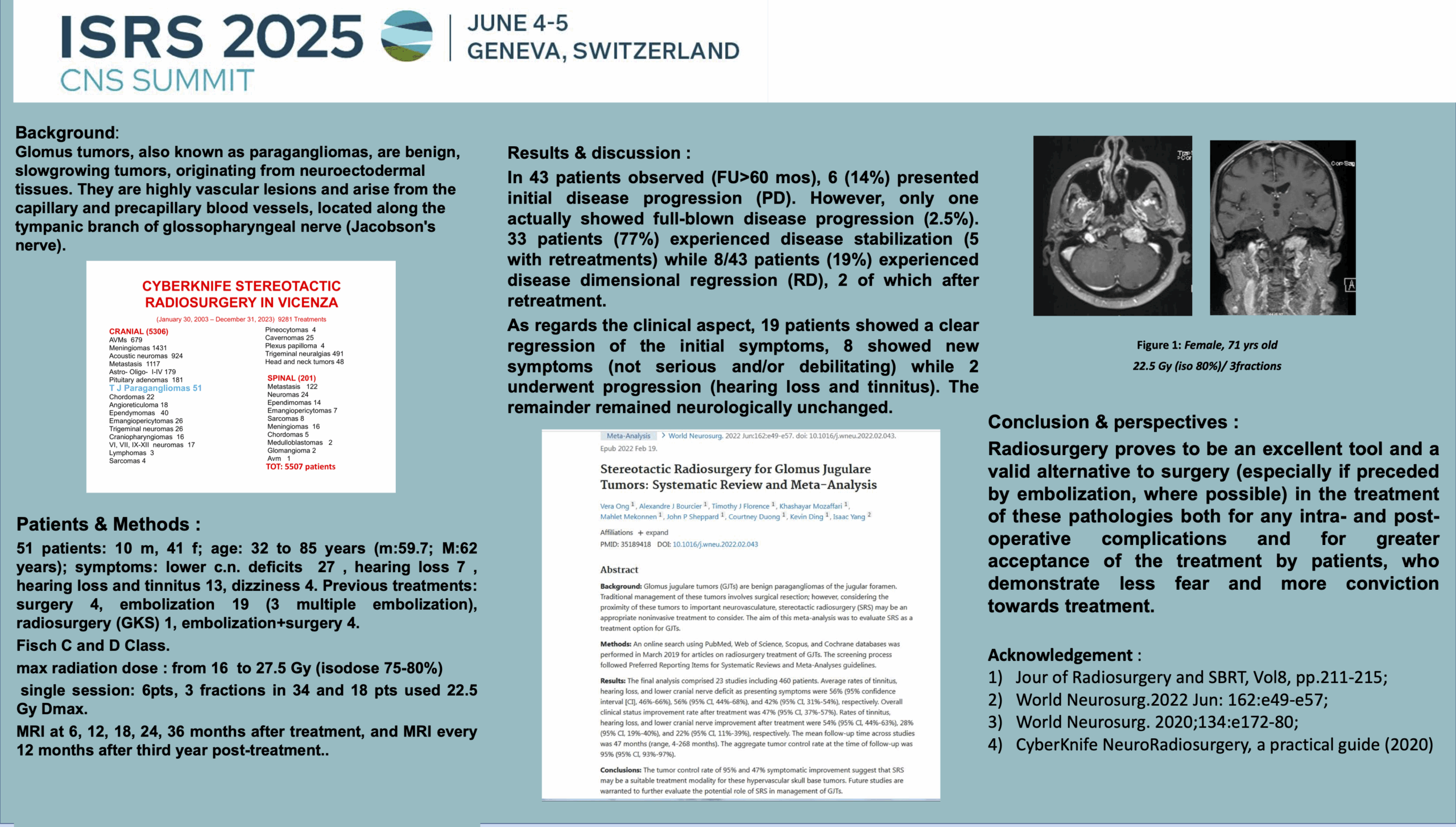
From January 2003 to December 2023, 51 patients (42 females and 10 males) affected by tympanojugular glomangioma were treated with CyberKnife at our Center.
The age ranged from 32 to 85 years (m: 59.7, M: 62). The average lesion volume treated was 4457 mm3 (median: 2660 mm3) while the range: 91-29331 mm3. Four patients showed multicentric lesions.
Six patients underwent 2 treatments and three underwent 3 treatments. while the maximum treatment doses delivered were between 16 and 27.5 Gy (average 21.3 Gy). The isodoses between 75-80%. In particular, a maximum dose of 22.5 Gy was used on 18 patients (34%). As regards fractionation, the majority of patients, 34/51, underwent three fractions while 6 underwent a single session.
No re-treatment was performed less than three years after the previous one.
The FU has a range of 5-150 months for a total of 2796 months of observation (average: 65).
43 patients underwent FU, 7 patients did not show up for checks while one died from senectus.
Radiological FU was scheduled at 6-12-18-24-30 and 36 months after treatment; 38 patients underwent checks with thin-layer contrast-enhanced MRI while the other 5 underwent high-definition contrast-enhanced CT due to no indication for MRI.
RESULTS
In 43 patients observed, 6 (14%) presented initial disease progression (PD). However, only one actually showed full-blown disease progression while five were re-treated. 27 patients (63%) experienced disease stabilization with a single treatment (SD) while 8/43 patients (23%) experienced disease dimensional regression (RD), 2 of which after retreatment.
As regards the clinical aspect, 19 patients showed a clear regression of the initial symptoms, 8 showed new symptoms (not serious and/or debilitating) while 2 underwent progression (hearing loss and tinnitus). The remainder remained neurologically quo-ante.